Wilson’s disease is a rare genetic disorder that disrupts the body’s ability to excrete excess copper. This condition leads to toxic copper buildup in critical organs like the liver, brain, and eyes. Although it is hereditary, early detection and proper management allow individuals to live healthy lives. Named after Dr. Samuel Alexander Kinnier Wilson, who first described it in 1912, this condition highlights the importance of genetic awareness and proactive healthcare.
Causes of Wilson’s Disease
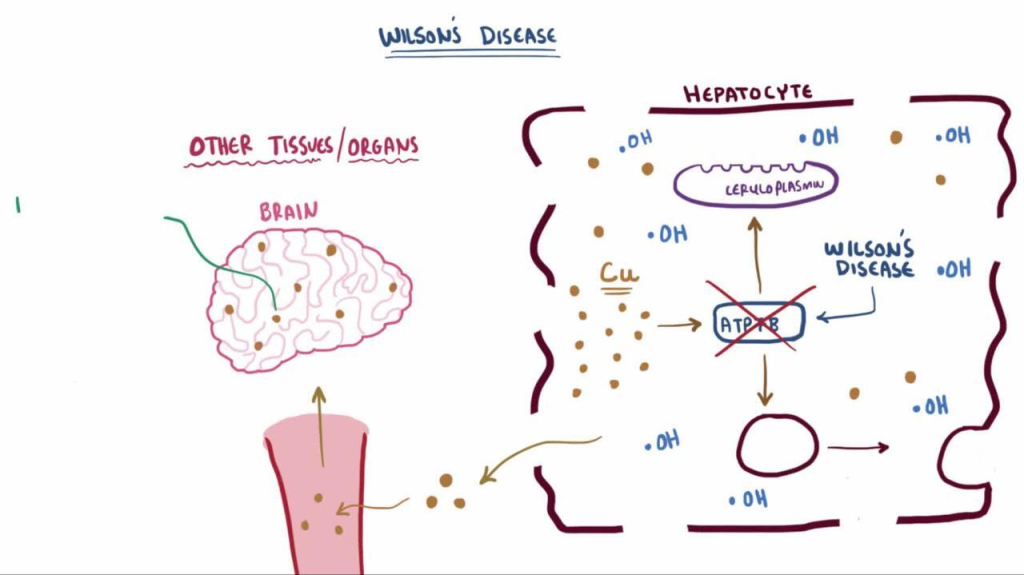
The primary cause of Wilson’s disease is a mutation in the ATP7B gene, which is responsible for regulating copper transport in the body.
Key factors include:
- Genetic Inheritance: The disease is autosomal recessive, requiring both parents to pass on the defective gene.
- Copper Imbalance: Failure to excrete copper leads to its accumulation in the liver, which eventually overflows into other organs, causing toxicity.
Indications of Wilson’s Disease
The early signs of Wilson’s disease can be vague, making diagnosis difficult without proper testing:
- Persistent fatigue and unexplained weakness.
- Jaundice or yellowing of the eyes and skin.
- Behavioral changes, including mood swings and depression.
- Abdominal swelling or pain.
Symptoms of Wilson’s Disease
Symptoms differ based on the organ affected:
- Liver Symptoms: Chronic hepatitis, cirrhosis, and acute liver failure.
- Neurological Symptoms: Tremors, muscle stiffness, speech difficulties, and unsteady gait.
- Psychiatric Symptoms: Anxiety, irritability, depression, and cognitive decline.
- Ocular Symptoms: Kayser-Fleischer rings, which are copper deposits around the cornea.
Prevention Strategies of Wilson’s Disease
While the genetic nature of Wilson’s disease means it cannot be fully prevented, certain strategies can help reduce complications:
- Genetic Testing: For families with a history of the disease, early testing can identify carriers or affected individuals.
- Regular Monitoring: Frequent tests for copper levels and liver function are crucial for at-risk individuals.
- Dietary Adjustments: Avoid foods high in copper, such as shellfish, nuts, and liver.
- Lifestyle Management: Following a structured treatment plan and adhering to medication schedules.
Myths and Facts About Wilson’s Disease
- Myth: Only adults develop Wilson’s disease.
Fact: Symptoms often begin in childhood or adolescence. - Myth: The disease is caused by a high-copper diet.
Fact: It is a genetic condition and not linked to dietary copper intake. - Myth: Only the liver is affected.
Fact: Wilson’s disease impacts multiple organs, including the brain and eyes.
Treatments and Therapy
Medication-Based Treatments
- Chelation Therapy: Medications like penicillamine or trientine bind copper, aiding its excretion through urine.
- Zinc Therapy: Blocks copper absorption in the digestive system and is used as maintenance therapy.
Surgical Treatments
- Liver Transplantation: Recommended for advanced liver damage when other treatments fail.
Physical Therapy and Rehabilitation
- Helps manage neurological symptoms like tremors and poor coordination, improving motor skills.
Lifestyle and Behavioral Interventions
- Following a low-copper diet and adhering to prescribed medications are critical for managing the condition.
Alternative and Complementary Medicine
- Techniques like yoga and meditation can help reduce stress and improve mental health but should complement standard treatments.
Psychotherapy and Counseling
- Provides emotional support to individuals and families coping with the challenges of a chronic illness.
Immunizations and Vaccines
- Protect against infections, especially in individuals with compromised liver function.
Stem Cell Therapy
- An experimental approach with potential for regenerating damaged liver tissue.
Gene Therapy
- Research is ongoing to correct the defective ATP7B gene, offering hope for a long-term cure.
Top 20 FAQ on Wilson’s Disease

1. What is Wilson’s disease?
A rare genetic disorder that causes toxic copper buildup in the liver, brain, and other vital organs.
2. How is it diagnosed?
Wilson’s disease is diagnosed through:
- Blood tests (e.g., ceruloplasmin levels).
- Liver function tests.
- Genetic screening.
- Eye examinations to detect Kayser-Fleischer rings.
3. What tests confirm the disease?
Key tests include:
- Serum ceruloplasmin levels.
- 24-hour urine copper levels.
- Liver biopsy to measure copper concentration.
4. Can it be cured completely?
There is no permanent cure, but lifelong treatments can effectively manage the condition and prevent complications.
5. Who is at risk?
Individuals with a family history of Wilson’s disease or those carrying ATP7B gene mutations are at higher risk.
6. Are there lifestyle changes needed?
Yes, necessary changes include:
- A copper-restricted diet.
- Avoiding high-copper foods like shellfish, organ meats, nuts, and chocolate.
- Adherence to prescribed medications.
7. What are Kayser-Fleischer rings?
Copper deposits around the cornea, visible during an eye examination, are a key diagnostic sign of Wilson’s disease.
8. How does it affect the brain?
Wilson’s disease can cause:
- Neurological symptoms like tremors, slurred speech, and poor coordination.
- Cognitive difficulties and psychiatric symptoms like depression and mood swings.
9. Can it cause infertility?
Yes, untreated Wilson’s disease may result in hormonal imbalances, potentially affecting fertility.
10. How is it managed during pregnancy?
Treatment continues with close monitoring. Medications like zinc therapy are prioritized to ensure safety for both mother and baby.
11. What is the role of zinc in treatment?
Zinc prevents copper absorption in the intestines and helps maintain safe copper levels in the body.
12. Are there home remedies?
Home remedies like following a copper-restricted diet and staying hydrated can complement medical treatment but cannot replace it.
13. What foods should I avoid?
Avoid copper-rich foods such as:
- Shellfish.
- Liver.
- Nuts.
- Chocolate.
- Mushrooms.
14. How long does treatment last?
Treatment is lifelong and requires consistent monitoring and adherence to medications and dietary recommendations.
15. What happens if untreated?
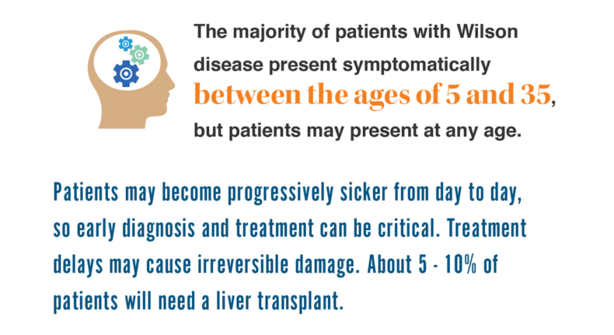
Without treatment, Wilson’s disease can lead to:
- Severe liver damage or failure.
- Neurological impairments.
- Death.
16. Can children develop it?
Yes, symptoms may appear in children as young as five years old, though they are often diagnosed during adolescence.
17. Does it cause fatigue?
Yes, fatigue is a common symptom due to liver dysfunction and the toxic effects of copper buildup.
18. Is genetic testing mandatory?
While not mandatory, genetic testing is strongly recommended for at-risk families to identify carriers and affected individuals early.
19. Are there new treatments available?
Research into gene therapy, advanced medications, and stem cell therapy is ongoing, offering hope for future treatment options.
20. Where can I get support?
Support is available through:
- Specialized medical centers and hepatologists.
- Advocacy organizations for rare diseases.
- Online communities and support groups for Wilson’s disease patients and families.
Conclusion
Wilson’s disease, though complex, is manageable with timely intervention, proper treatments, and lifestyle modifications. Spreading awareness about the condition can improve outcomes and prevent severe complications. If you or a loved one have a family history or symptoms of Wilson’s disease, seek medical advice for early diagnosis and management.
Take charge of your health and live a full life with the right support and care!
Related video: